UDI TIME SCHEDULES.
Apply for a Labeler Identification Code (LIC).
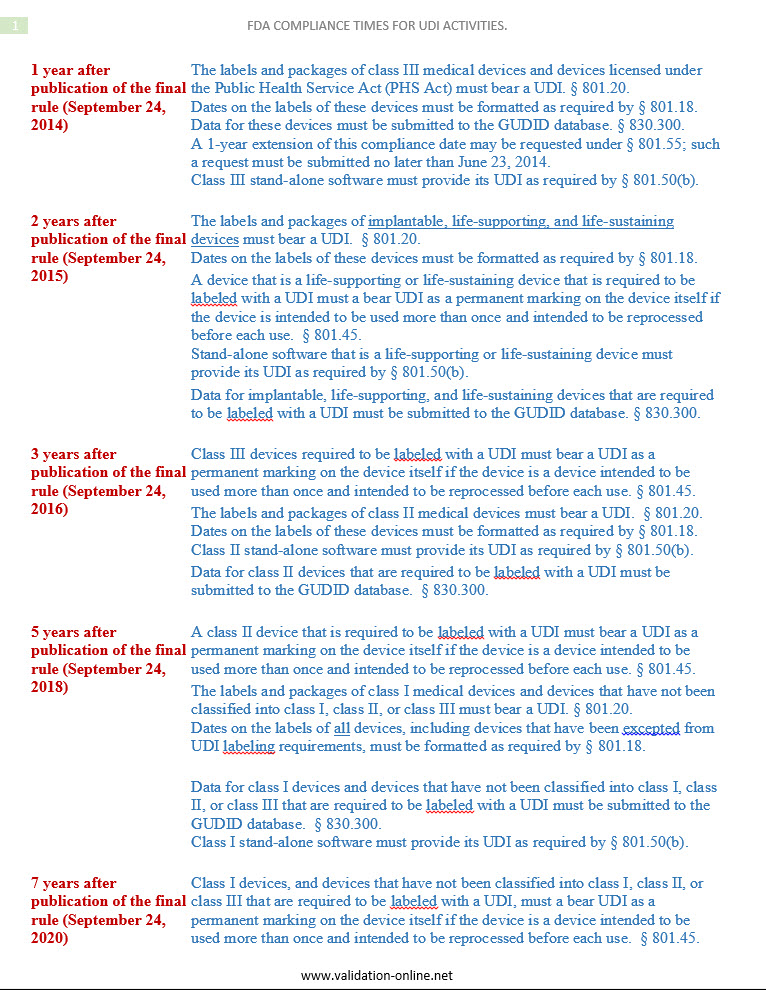
The UDI Time Schedules has identified the Health Industry Bar Code Supplier Labeling
Standard (HIBC SLS) as a data standard for UDI. The FDA regulation
requires a product identifier, as well as a labeler identifier.
UDI Time Schedules Questions and Answers.
- Does my device require the “direct marking” of the UDI number? This depends on the type of device, as all medical devices intended to be used more than once or intended to be reprocessed before each use must have direct marking of the UDI. The FDA has stated as part of the regulation that implantable devices will not require the direct marking. Single-use devices do not require direct marking of the UDI number on the device.
- What packaging level do I need to place the UDI on the labels?
The UDI must be on each level of packaging up to shipping, which does
not require the UDI number to be on the shipping box or pallet. The
important thing to remember is that the UDI must be available to the
user at all points of use. As an example, a carton of ten units sitting
on a shelf must have the UDI number, and the individual unit from that
carton being used at the patient bedside must have the UDI number. UDI time schedules historical notes.
- Where do I actually get this UDI number? There are
three Issuing Agencies (IA) currently accredited by the FDA that assign
the Device Identifier portion of the UDI. The Device Identifier (DI) is
composed of a unique company identification and a unique number
assigned to each version or model of device. If a company has ten
different models or versions of a device, then they would have 10
distinct DI numbers. The UDI may then be composed of the DI and the
Production Identifier (PI) that includes information such as lot number,
serial number, or expiration date. The FDA does not actually assign the
UDI since this number is obtained from the IA and then entered into the
FDA’s Global Unique Device Identification Database (GUDID). UDI time schedules guidance.
- How do I get an account with the FDA for the GUDID database? Currently the FDA is only assigning GUDID accounts after these are requested through an email request from the FDA. That is, a firm must request a GUDID account on the FDA website; the FDA then sends the applicant a form to fill out. Once the applicant sends back the form to the FDA via email, the agency reviews the form, and then sends an email back to the applicant with GUDID account log-in information. In other words, it’s not like other sites where one can just “register” to set up an account. The FDA is limiting the amount of accounts being assigned currently in order to manage and build the GUDID system. Only Class III, life-sustaining, and life-supporting devices are being provided GUDID accounts. No Class II or Class I devices are able to obtain a GUDID account at this time. However, this does not preclude that companies can already obtain their DI number through the Issuing Agency and start placing the UDI on their packages; they just would not be able to enter the information in the FDA GUDID database yet.
- Do we need to change the date format on our labeling?
The FDA has specified in the regulations that the date format of
YYYY-MM-DD must be used for all dating on product labeling such as
expiration dates or date of manufacture. If an organization is currently
using the MM-DD-YYYY or MM-YYYY format for their expiration dating,
then this would need to be changed to stay compliant with the
regulations. UDI time schedules historical notes.
- There are many types of bar codes that exist; which one am I required to use? The FDA has made it clear that Automatic Identification and Data Capture (AIDC) such as bar codes are “technology neutral,” meaning that whichever method a Labeler/Manufacturer chooses, there is technology that can be used. An organization must determine which bar code or other AIDC technology is most appropriate for their device and their customer needs. As an example, a Class III device with a long UDI number and a small package may need to consider a 2-D Matrix style bar code in order to fit on the label. Or a Class II device with a large label being sold in small doctors’ offices with limited bar code reader capability could choose to use a GS1-128 style linear bar code on the package label.
- I have my UDI, is that all or are the other things that I need to do?
As with any regulatory compliance, there always seems to be an endless
chore of activities that need to be performed. The quality management
system must be updated to include all of the requirements associated
with UDI number management. This includes when packaging or labeling is
changed that the Change Order process must have an assessment or impact
evaluation to continue compliance with the regulations. The customer
complaint and adverse event procedures must ensure that they are
capturing the UDI information. An overall procedure or process should be
documented for how the UDI numbers are managed, including steps for
obtaining the number, adding new versions or models, and discontinuing
versions or models. It is advisable that the UDI process is integrated
into the entire quality management system as it can touch on many areas
such as labeling, supplier management, Device History Records, customer
complaints, and recall activities. UDI time schedules guidance notes.
This article originally appeared on www.emergogroup.com.